 Vasa previa is an obstetrical condition in which fetal vessels cross over the internal cervical os. The cervical os is the opening from the womb to the birth canal, and is through which the baby is delivered vaginally. Because the vasa previa vessels are unsupported by underlying placenta, these vessels may be damaged if the bag of waters breaks or if the cervix dilates (opens) during labor. These vessels are directly connected to the baby. If these vessels break open, it can result in sudden blood loss and drop in blood pressure of the baby.
Vasa previa is an obstetrical condition in which fetal vessels cross over the internal cervical os. The cervical os is the opening from the womb to the birth canal, and is through which the baby is delivered vaginally. Because the vasa previa vessels are unsupported by underlying placenta, these vessels may be damaged if the bag of waters breaks or if the cervix dilates (opens) during labor. These vessels are directly connected to the baby. If these vessels break open, it can result in sudden blood loss and drop in blood pressure of the baby.
Vasa previa has historically been associated with high perinatal mortality rates due predominantly to fetal hemorrhage (bleeding) after vessel damage at time of membrane rupture. However, there has been a significant reduction of the perinatal mortality rate. This may be attributed to intensive monitoring of the pregnancy and subsequent preterm elective cesarean section timed to precede rupture of membranes.
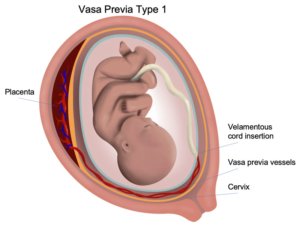
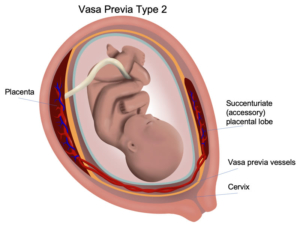
Vasa previa has been classified into two types: Type I if the vasa previa arises directly from a velamentous umbilical cord insertion, and Type II if it bridges separate lobes of a bilobed or succenturiate placenta. Diagnosis and classification of a vasa previa is feasible by ultrasound evaluation of the lower uterine segment. Often endovaginal ultrasound will be
necessary to confirm the diagnosis.
 Patients with Type II Vasa Previa may be offered the following treatment options:
Patients with Type II Vasa Previa may be offered the following treatment options:
- Expectant management: The perinatal mortality rate for vasa previa has been historically quoted to be upwards of 40 to 50% due to unrecognized rupture of the fetal vessel and resultant fetal exsanguination. The perinatal mortality rate for prenatally recognized vasa previa may be as low as 3%. The rate of perinatal morbidity is unknown. Hospitalization for the duration of the pregnancy is usually recommended between 28 and 32 weeks gestation to maintain close proximity to the operating room in case of suspected rupture of the vasa previa. Because about one-third of patients may develop vaginal bleeding during the course of the pregnancy, timely identification of the source of bleeding and access to continuous fetal monitoring is required. Corticosteroids at 28 weeks for fetal maturation therapy is often given. Delivery is recommended without prior amniocentesis at 35 weeks gestation.
- Operative fetoscopy and laser ablation of the vasa previa. The potential benefit of this option is that risk of sudden fetal death from rupture of the vasa previa is substantially less. This option would also remove the diagnostic dilemma of vaginal bleeding. Prolonged hospitalization may be avoided, and delivery may occur beyond 35 weeks gestation. The risks of this option are those related to operative fetoscopy in general, such as preterm rupture of membranes and preterm labor.
For further reading, please see the link below: